Chronic pain, defined as persistent pain extending beyond the normal healing period, poses significant challenges for patients and clinicians alike. Traditional treatments, particularly opioids, are associated with dependency, tolerance, and adverse side effects. Increasingly, alternative therapies such as cannabinoids, psilocybin, and ketamine are emerging as potential tools to manage complex and recurrent pain conditions.
Cannabinoids: A Natural Pain Modulator
Cannabis-derived compounds, particularly tetrahydrocannabinol (THC) and cannabidiol (CBD), act on the body’s endocannabinoid system to influence pain perception. Recent studies have highlighted their role in treating chronic pain associated with conditions like neuropathy, fibromyalgia, and multiple sclerosis.
A randomized trial using low doses of THC demonstrated significant pain reduction, with 39% of patients experiencing improvement compared to placebo. Another study observed improved sleep quality and reduced pain scores in fibromyalgia patients treated with cannabis-based formulations.
Long-term use of cannabinoids may increase the risk of mild to moderate adverse effects, including dizziness and drowsiness. Moreover, high-potency THC has been linked to a higher risk of psychosis, necessitating careful patient selection and dosage management.
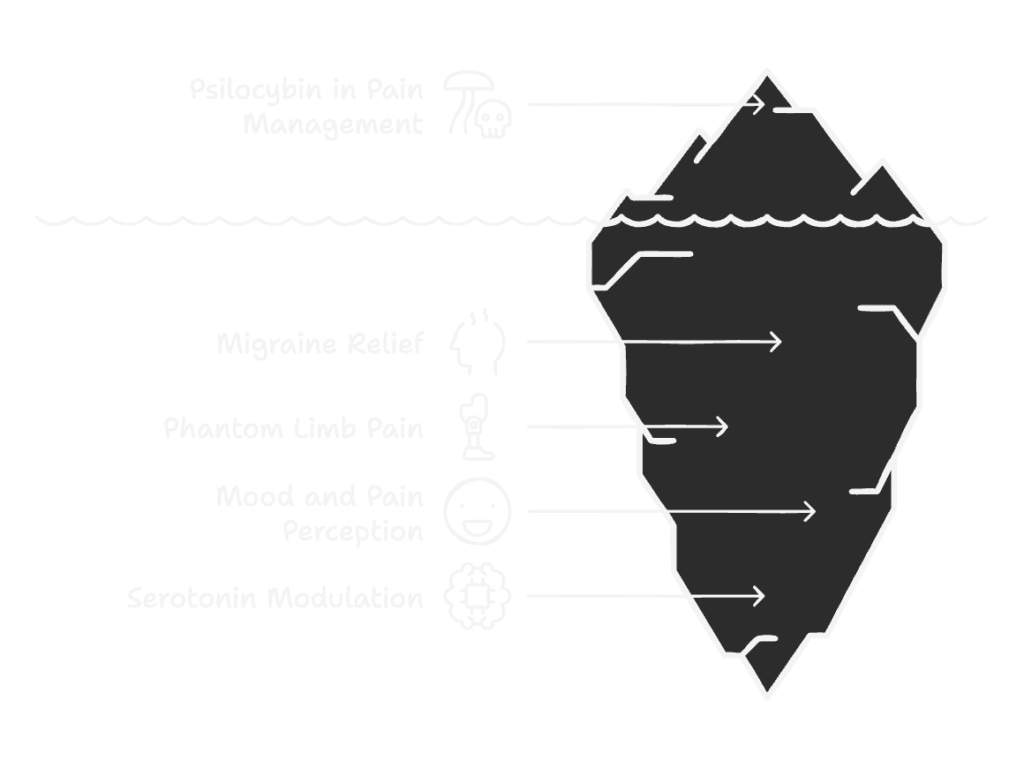
Psilocybin: The Psychedelic Pathway
Psilocybin, a serotonergic hallucinogen found in “magic mushrooms,” acts primarily on 5-HT2A receptors. Its ability to alter functional brain connectivity has implications for pain modulation, particularly in conditions like migraines and phantom limb pain.
Mechanisms of Action
Psilocybin’s interaction with serotonin receptors leads to altered functional connectivity in the brain. This process can disrupt maladaptive pain pathways and help rewire the brain’s perception of pain. Functional magnetic resonance imaging (fMRI) studies have shown that psilocybin reduces activity in the default mode network (DMN), a brain network implicated in chronic pain conditions and mood disorders. By modulating activity in the DMN and other neural circuits, psilocybin can potentially change how pain is processed and experienced.
Additionally, psilocybin’s effects on neuroplasticity are noteworthy. It has been shown to activate pathways involved in neuronal growth, such as the mammalian target of rapamycin (mTOR) and tropomyosin receptor kinase B (TrkB) pathways. These mechanisms may underlie its ability to “reset” maladaptive neural connections, making it particularly useful for conditions characterized by central sensitization, such as fibromyalgia and phantom limb pain.
Clinical Evidence and Case Studies
Although large-scale studies are lacking, early research and anecdotal reports highlight psilocybin’s potential:
- Migraine Relief: Psilocybin shares structural similarities with triptans, a class of medications used for migraines. Initial studies suggest that psilocybin can reduce the frequency and severity of migraine attacks by modulating serotonin pathways involved in pain perception.
- Phantom Limb Pain: A case report detailed the use of psilocybin in a patient experiencing intractable phantom limb pain following amputation. When combined with mirror visual feedback therapy—a method that tricks the brain into perceiving the absent limb as present—psilocybin led to a complete resolution of pain and reduced paroxysmal episodes. This synergistic effect underscores the compound’s potential for treating complex neuropathic pain conditions.
- Mood and Pain Perception: Psilocybin’s ability to alleviate anxiety and depression may also contribute to its efficacy in pain management. Chronic pain often exacerbates psychological distress, creating a feedback loop that intensifies suffering. By improving mood and reducing stress, psilocybin indirectly helps patients cope with their pain more effectively.
Despite its promise, psilocybin faces several hurdles:
- Limited Research: Most studies on psilocybin and pain are small and exploratory. Larger, controlled trials are needed to establish efficacy and safety.
- Side Effects: In clinical trials, some participants reported transient side effects such as nausea, dizziness, and headaches. Psilocybin also induces hallucinogenic effects, which may not be suitable for all patients.
- Regulatory Barriers: As a Schedule I substance in many countries, psilocybin remains heavily restricted. This status limits research and complicates access for therapeutic use.
Future Directions
Ongoing studies aim to expand the evidence base for psilocybin in pain management. Key areas of focus include:
- Chronic Pain Syndromes: Investigating its role in fibromyalgia, cluster headaches, and neuropathic pain.
- Combination Therapies: Exploring synergistic effects when combined with cognitive-behavioral therapy (CBT), physical rehabilitation, or other pharmacological agents .
- Microdosing: Assessing whether low, sub-hallucinogenic doses of psilocybin can provide therapeutic benefits without altering consciousness.
Psilocybin represents a novel approach to pain management by addressing both the psychological and physiological components of chronic pain. While its hallucinogenic properties may pose challenges, its potential to reset neural circuits and modulate pain perception warrants further investigation. As regulatory landscapes evolve and research progresses, psilocybin could become a valuable tool in the arsenal against chronic and recurrent pain.
Ketamine: A Disruptor of Pain Pathways
Ketamine, an NMDA receptor antagonist, offers rapid pain relief by disrupting maladaptive neuronal circuits. Its efficacy in treating neuropathic pain and complex regional pain syndrome has been well-documented.
Ketamine promotes neuroplasticity and reduces central sensitization, resetting dysfunctional pain pathways. Its use as a dissociative anesthetic adds a unique dimension to pain management.
Studies have shown ketamine’s potential in providing sustained analgesia for patients unresponsive to traditional therapies. However, its dissociative effects and potential for misuse remain concerns.
Conclusion
Cannabinoids, psilocybin, and ketamine represent a paradigm shift in chronic pain management, offering hope for patients with complex pain syndromes. While their mechanisms differ, these compounds share the potential to modulate pain perception and improve quality of life. Robust, large-scale studies are essential to establish their efficacy, safety, and optimal application in clinical practice.


